Have you ever walked out of a psychiatric appointment wondering if you were truly heard? Maybe you barely had time to explain what you’re feeling before a prescription was pushed your way. If that sounds familiar, you’re not alone.
Welcome to Drive-Thru Psychiatry
Mental health care in the United States has been reduced to what can only be described as drive-thru psychiatry.
More and more people walk into a clinic, spend a mere 15 minutes with a provider, receive a diagnosis, leave with a prescription (or both), and leave confused about what just happened. These rushed visits aren’t rare.
They’ve become the standard in our corporatized mental healthcare system.
And for people with layered health concerns, trauma histories, or complex diagnoses, this model is not just inadequate — it’s dangerous.
What Can Really Happen in 15 Minutes?
Let’s be honest: not much.
Yet, 15 minutes is the standard length of most psychiatric appointments in many major health systems and corporate-run clinics.

What can you do in that time? Maybe skim a checklist. Maybe talk about one symptom. But what you can’t do is understand someone’s trauma history, family dynamics, medical background, or side effects from previous treatments.
In short, you can’t see the person. And the system doesn’t seem to care. It rewards speed.
As research by Ahmed (2023) confirms, both patients and providers know these visits are not enough, especially for those with ongoing or complex mental health concerns.
The Corporate Takeover of Mental Health
Behind this rushed care is a deeper issue, a business model that now dominates medicine: corporatization.
Clinics and hospitals are increasingly owned by private equity firms, insurance companies, and large healthcare conglomerates. These entities prioritize volume over value, which means more patients, shorter visits, and protocol-driven treatment plans that leave little room for nuance.
A study by Malâtre-Lansac et al. (2020) reveals that psychiatrists in corporate-owned practices are pressured to hit productivity metrics. They’re expected to see as many patients as possible in the shortest time.
The result? Patients become numbers. Visits become check-ins. Medication becomes the default.
The Cost of Quick Diagnoses and Default Prescriptions
When mental health care is reduced to a quick diagnostic checklist, patients pay the price. Misdiagnosis is far too common, especially with nuanced conditions like complex PTSD, ADHD, bipolar II disorder, and somatic symptoms.
These diagnoses require time, trust, and conversation to get right.
But in many of today’s rushed appointments, patients are handed a label and a prescription—with little to no explanation, no space to ask questions, and no discussion of alternatives.
Too often, side effects go undiscussed. Long-term risks are glossed over. And many people don’t even realize that options like psychotherapy, trauma-informed care, or integrative treatments exist.
As Yager et al. (2022) point out, “medication management” has become the core function of modern psychiatric visits. But prescribing without understanding isn’t care—it’s pharmaceutical triage. And it leaves too many people feeling misdiagnosed, overmedicated, and unheard.
Real Stories, Repeated Struggles
I see the same heartbreaking pattern every day. Clients come to me after being misdiagnosed, medicated without true informed consent, or bounced from provider to provider—never truly heard, never truly seen.
Many arrive feeling disoriented, ashamed, and unsure if their symptoms are actually being treated or just temporarily silenced.
These aren’t rare cases—sadly, they’re the norm in today’s broken system.
And that’s exactly why I created Before You Medicate – LIVE to help people pause, get informed, and take back control before agreeing to a diagnosis or prescription they don’t fully understand.
Before You Medicate – LIVE
If you’ve ever walked out of a psychiatric appointment feeling confused, unsure, or even dismissed, this workshop is for you.
Before You Medicate – LIVE is a transformative, guided workshop I created to give you the clarity, tools, and confidence you need before saying yes to a diagnosis or prescription you don’t fully understand.
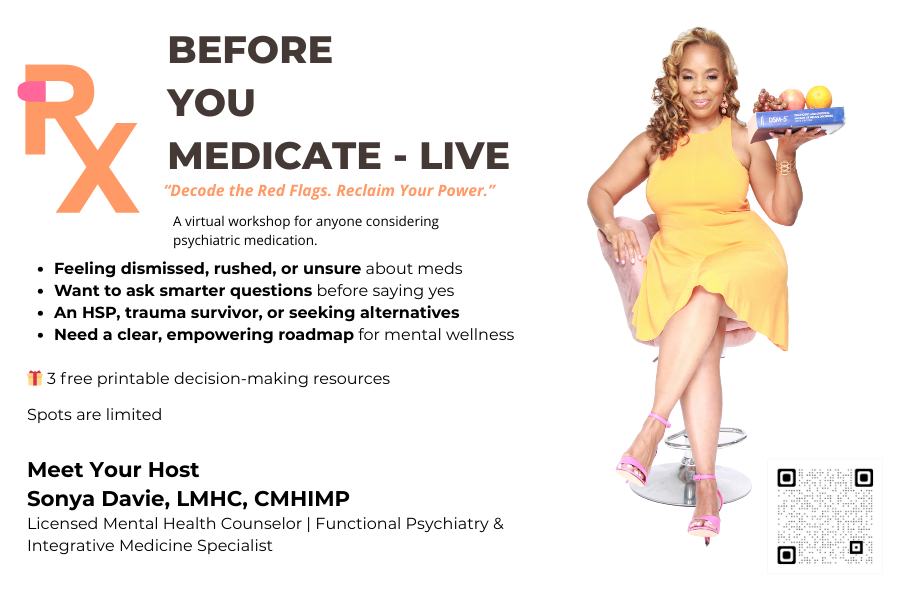
Because when it comes to your mind and body, informed decisions aren’t optional—they’re essential.
In this workshop, you’ll learn:
- How psychiatric diagnoses are made—and how they’re sometimes misapplied
- The key questions to ask before agreeing to a medication
- How to explore non-medication and integrative treatment paths
- Language to confidently advocate for yourself or a loved one
- That you have options—and a right to understand them
This workshop is not anti-medication. It’s pro-choice, pro-inquiry, and pro-patient empowerment. Because you deserve to be seen, not rushed.
You Deserve More Than 15 Minutes!
Short psychiatric visits aren’t a solution—they’re a symptom of a broken system that values billing codes over human beings. Patients aren’t problems to be solved in 15 minutes. They are complex, layered individuals with stories, trauma histories, and needs that deserve time, attention, and respect.
Mental health isn’t a quick fix. It’s a journey that requires care, curiosity, and collaboration. And we can’t keep waiting for the system to change—we have to change how we engage with it.
That starts with education. By asking better questions. With expecting better answers.
If you’re ready to take that first step, join me for Before You Medicate – LIVE , a workshop designed to empower you with clarity, confidence, and real options.
Because your mind—and your story—deserve more than 15 minutes.
References
- Ahmed (2023) – Stakeholder Views on Short Psychiatric Visits
- Yager et al. (2022) – The Dominance of Medication Management in Psychiatry
- Malâtre-Lansac et al. (2020) – Corporate Pressures in Behavioral Health Care
+ show Comments
- Hide Comments
add a comment