Diabetes is often viewed as a physical illness, yet it’s deeper… More intricate roots frequently lie within the psyche. Emerging research reveals powerful links between trauma, mental health, and diabetes.

Conditions such as depression, anxiety, post-traumatic stress disorder (PTSD), and adverse childhood experiences (ACEs) don’t just shape our emotions; they can disrupt the body’s entire stress-response system, influencing metabolism, inflammation, and blood sugar regulation.
These connections aren’t coincidental… They highlight the complex, bidirectional relationship between the mind and metabolism.
Related Post: Diabetes Awareness Month: How Blood Sugar Imbalance Can Affect Mental Health
The Historical Roots of a “Depressogenic” Disease
The link between emotional distress and diabetes isn’t new. As far back as the 17th century, physician Thomas Willis described diabetes as arising from “long sorrow and other depressions.” In 1879, psychiatrist Sir Henry Maudsley observed that diabetes often appeared in families where mental illness was common, remarking that “diabetes is a disease which often shows itself in families in which insanity prevails.” (Source)
Today, diabetes is often described as a “depressogenic” illness — one that both contributes to and is worsened by depression. Research consistently supports this two-way relationship.
Adults living with depression are about 60% more likely to develop diabetes. Conversely, individuals already diagnosed with diabetes (type 1 or type 2) are twice as likely to experience major depressive disorder compared to the general population. (Source)
These findings reflect what many people already sense intuitively: when emotional pain remains unprocessed, the body often carries it too.
This underscores how deeply interconnected mental and metabolic health truly are.
PTSD, Anxiety Disorders, and Metabolic Dysfunction
Trauma-related conditions like PTSD are increasingly recognized as risk factors for developing diabetes. Symptoms such as chronic hypervigilance, disrupted sleep, anxiety, and emotional dysregulation can keep the body in a prolonged state of stress. Over time, this constant activation of the stress-response system can impair insulin sensitivity and disrupt blood sugar balance.
In fact, anxiety disorders are reported to be three times more common in people with diabetes, and overlapping symptoms such as fatigue, irritability, and restlessness can blur the lines between high blood sugar and anxiety, making diagnosis and management more challenging.
Adverse Childhood Experiences (ACEs): The Early Roots of Chronic Disease
Adverse Childhood Experiences or ACEs include experiences such as abuse, neglect, and household dysfunction (like witnessing violence, parental separation, or growing up around substance misuse).
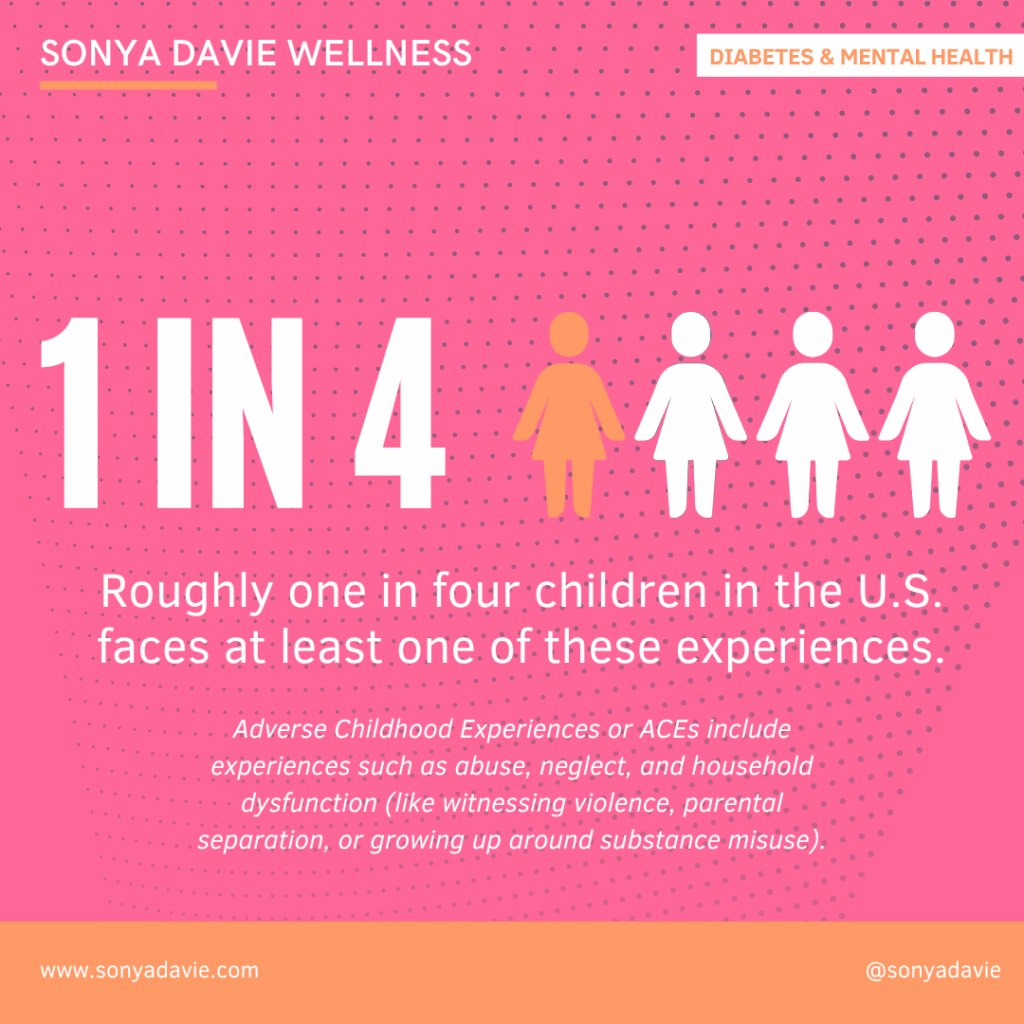
Research shows that ACEs have a dose-response relationship with chronic disease risk in adulthood.
A review found that adults who experienced four or more ACEs have about a 52% higher risk of developing diabetes than those with none. (Source)
Another meta-analysis found that additional ACE increases diabetes risk by approximately 5%. (Source)
Why? Because chronic early stress can dysregulate the hypothalamic-pituitary-adrenal (HPA) axis, leading to increased cortisol and inflammation of which fuel insulin resistance over time.
Simply put, when the body learns early to stay in survival mode, that pattern can persist into adulthood, setting the stage for metabolic changes that increase the risk of diabetes.
The Immune‑Inflammatory Bridge: hs‑CRP, Depression & Diabetes
Inflammation connects the dots between depression and diabetes. High-sensitivity C-reactive protein (hs-CRP), a marker of systemic inflammation, has been found to be higher in individuals living with both conditions.
In one study, older adults with both depression and diabetes faced more than double the mortality risk compared to those with just one of the two conditions. Elevated hs-CRP levels were a key factor in that increased risk, underscoring how inflammation, mood, and metabolism are intricately intertwined. (Source)
When the immune system remains activated for too long, it not only affects physical health but also increases emotional vulnerability and fatigue.
This highlights how the combination of metabolic disease, mood dysregulation, and inflammation magnifies risk far beyond any single condition.
Clinical Implications: The Need for Trauma-Informed, Integrative Care
Understanding these multi-layered links between trauma, mental health, and metabolic function is essential for improving outcomes. A trauma-informed, integrative approach acknowledges that physical symptoms often have emotional roots and that both need to be addressed for true healing.
Key considerations for practitioners and patients alike:
#1 – Routine screening for depressive and anxiety symptoms in patients with diabetes (and vice versa).
#2 – Probing the history of ACEs, chronic trauma or PTSD when metabolic issues are present.
#3 – Recognizing that hyperglycaemia and anxiety may share symptom overlap necessitates a thoughtful differential diagnosis.
#4 – Targeting lifestyle interventions (nutrition, movement, sleep, stress‑reduction) that support both metabolic and mental health.
#5 – Monitoring inflammatory markers (e.g., hs‑CRP) as part of a broader assessment in complex cases.
#6 – Bringing in trauma‑sensitive psychotherapy, mindfulness, and stress‑modulation practices as adjuncts to standard endocrine/metabolic management.
Why This Matters for You
If you are navigating trauma, depression, anxiety, or a metabolic condition like diabetes, please know this: these are not separate struggles. They are connected expressions of the same stress-response system trying to find balance.
Diabetes is not simply a “blood sugar problem.” It’s also a psychological and developmental condition influenced by life experiences, stress patterns, and emotional regulation.

When we treat the body while ignoring the mind, or the mind while neglecting the body, we miss half the story.
For individuals who have experienced early adversity, chronic stress, or mental health challenges, it’s essential to recognize their heightened vulnerability to insulin resistance, diabetes onset, and poorer outcomes.
Integrating emotional healing, mental wellness, stress reduction, and trauma-informed support into metabolic health programs isn’t optional — it’s foundational for long-term wellness.
In Summary
- Depression increases the risk of developing diabetes by roughly 60%.
- People with diabetes are twice as likely to experience major depression.
- PTSD and chronic anxiety symptoms significantly raise the risk of metabolic dysfunction.
- Elevated hs-CRP in individuals with both diabetes and depression predicts poorer outcomes.
- Each additional Adverse Childhood Experience increases adult diabetes risk.
- A trauma-informed, integrative approach that addresses stress regulation, inflammation, mental health, and lifestyle is key to better outcomes.
+ show Comments
- Hide Comments
add a comment